Preparedness for the next pandemic: the international community gears up
The risk of new pandemics is increasing. The main causes are environmental destruction, global warming and increasing globalization. The international community sees a need to prepare jointly and effectively for future pandemics. The G7 countries have taken the initiative together with the World Health Organization and other UN agencies, involving research institutions and research-based medicine manufacturers: In a "Pact for Pandemic Readiness".

The need for such an international pact arises, on the one hand, from the enormous damage caused by a pandemic: 6.3 million deaths worldwide, 530 million confirmed infections, consequential health damage (long covid) and, as a result of lockdowns, a sharp decline in economic output, disruption of international supply chains, and massive long-term damage to children and young people as a result of daycare and school closures. On the other hand, the probability of occurrence of future pandemics increases: Hamburg virologist and tropical medicine expert Professor Jonas Schmidt-Chanasit (1) points to the clear link between global environmental degradation and global warming and the emergence of new infection threats to humans. He cites examples:
- Ebola was partly caused by massive human intervention in the habitat of wild animals through the establishment of plantations or factory farms. Pathogens that normally live in closed ecosystems then manage to jump to humans the livestock.
- Warmer spring and summer months in Germany have led to zoonotic pathogens transmitted by mosquitoes on the rise in regions that were previously too cold. One example is the Usutu virus, of which an "intensive increase" is observed in Germany by way of transmission by mosquitoes. Blackbirds are mainly affected, but in immunocompromised people the virus can cause meningitis.
New risk: Global warming
Because climate change is a reality and the transmission of viruses to humans can hardly be prevented in a globalized world and due to necessary social contacts, Schmidt-Chanasit says that in the future, the response must be much faster than in the case of the Sars-CoV-2 pandemic. This will require concerted international action by many stakeholders:
- the World Health Organization, together with other UN agencies such as the Food and Agriculture Organization (FAO), the UN Environment Programme (UNEP) and the World Organisation for Animal Health (OIE),
- the national governments,
- research institutions and the research-based pharmaceutical industry.
In a "One-Health-in-All" approach. This means that a strategy for pandemic readiness must involve all policy areas: environment, economy, labor, and education, in addition to health.
In the meantime, several dozen initiatives have been formed that - depending on their expertise - aim to detect and monitor disease outbreaks early, provide a rapid, decisive and coordinated response to health threats, and develop tests, vaccines and therapeutics. The "G7 Pact for Pandemic Readiness", which aims to significantly strengthen the role of the WHO and coordinate the diverse activities and initiatives, is of great importance in this context. (2)
Thus, at their conference in Berlin on May 19th and 20th, the G7 health ministers reaffirmed their intention to "strengthen the agility of the WHO" and increase the mandatory contributions.
Collaborative Surveillance: Early Detection and Surveillance
The goal is to significantly increase the speed of response to emerging pandemics through systematic global monitoring. The WHO is to be put in a position to proactively and immediately publicize critical epidemiological warning signs. The Global Hub for Pandemic and Epidemic Intelligence, established in Berlin in September 2021, will play an important role in this regard, acting as a global hub for pandemic-related data generation and analysis. The goal is to have a global data ecosystem available "from which important action-oriented insights will emerge for governments and those responsible" (German Chancellor Angela Merkel in May 2021).
Other Collaborative Surveillance program items include:
- The formation and support of cross-sectoral genome sequencing networks to identify new variants and pathogens early in their emergence in humans, animals and the environment - an essential prerequisite for the development of testing methods, vaccines and therapeutics;
- Strengthening geographically dispersed centers of excellence in the global North and South;
- improving structured education and training networks with up-to-date curricula and common standards;
- Improving networks for consultation among peers;
- breaking down barriers that prevent rapid cross-border and cross-sector sharing of data and samples.
Predictable Rapid Response.
Based on better, up-to-date global surveillance, combined with strengthened and broadened expertise, rapid and reliable crisis responses are to be implemented in the future as a "decisive and coordinated response to health threats" (G7 objective). Important points here are:
- Establishing and supporting professional and well-trained "readinesss teams" that are integrated into local disease surveillance and response systems and are familiar with regional or local conditions;
- increasing WHO's own technical crisis response capacity; this includes promoting the Global Outbreak Alert and Response Network, which includes more than 200 institutions such as the U.S. Center of Disease Control, the Robert Koch Institute in Germany, UNICEF, and Doctors Without Borders, which make their expertise available in crisis regions worldwide;
- Supporting research and development of tests, vaccines and therapeutics, building regulatory capacity and production capabilities.
The G7 countries are committed to further accelerating research and development and advocate the voluntary transfer of technology and know-how. The goal is the safe approval and fastest possible and equal availability of new interventions such as vaccines, diagnostics and therapeutics. The experience gained in vaccine and diagnostics development and approval during the Covid 19 pandemic is to be used in this context. It will also support the expansion of research and manufacturing capacity in low- and middle-income countries and related industry efforts.
Later this year, as a result of a third conference, the G7 countries, together with the World Health Organization and key stakeholders and experts, intend to adopt a "Roadmap for Practical Cooperation."
A plethora of initiatives for future pandemic defense
Against the backdrop of the Covid 19 pandemic, a plethora of new institutions and initiatives have emerged over the past two years at the national and international levels by governments, researchers and industry. At the heart of these is their collaborative, cross-sector and cross-disciplinary approach with the goal of responding more quickly and effectively to future, more likely pandemics caused by new pathogens. Some key projects at a glance:
Coalition for Epidemic Preparedness Innovations (CEPI).
CEPI, the Coalition for Epidemic Preparedness Innovations, was initiated due to inadequate preparations for the 2014 Ebola fever epidemic and the 2015/16 Zika virus epidemic at the World Economic Forum in Davos in January 2016 and formally established a year later. Founding members were Norway, India, Germany, the UK Wellcome Trust, and the Bill and Melinda Gates Foundation. The main goal is to develop vaccines that align with the WHO priority list and support technical platforms that can act quickly when new epidemics emerge. As part of the Covax initiative, CEPI also advocates for equitable access to vaccines for developing countries. The funding goal is $3.5 billion.
Pandemic Preparedness Partnership (PPP)
Initiated by the British government. The goal here, too: Through cooperation among industry, international organizations and leading scientists, to have vaccines, diagnostics and therapeutics available 100 days after an international health emergency is declared.

The initiative, which emerged in May 2021, has been endorsed by the G7 Summit (Cornwall 2021) and the G20 2021 meeting. First steps: the establishment of a Global Pandemic Data Alliance and collaborations between industry and research institutes on platform technologies such as mRNA or viral vectors. This year, a decision will be made on which virus families should be the focus of prototype vaccine development. To this end, it should be possible to estimate how likely a particular virus family is to produce the causative agent of a new disease X for humans. This will be followed by a priority list defined jointly with the WHO.
WHO Hub for Pandemic and Epidemic Intelligence
Established in Berlin in September 2021, the hub will use artificial intelligence to provide datasets on topics such as animal health, the occurrence of unusual diseases in humans, the link to climate change model calculations for risk assessment, enabling early countermeasures. Experience from previous pandemics and epidemics will be incorporated.
Initiatives for the development of diagnostics and therapeutics
The Intrepid Alliance brings together research-based pharmaceutical companies to work with non-profit organizations to develop 25 oral therapeutics to completion of Phase I clinical trials (testing in healthy individuals) within five years.
The Pandemic Antiviral Discovery initiative is supported by the Novo Nordisk Foundation, Open Philanthropy and the Bill & Melinda Gates Foundation. The goal is to explore prioritized virus groups, identify therapeutic targets in three of these virus groups and develop compounds to Phase I.
The National Alliance for Pandemic Therapeutics (NA-PATH) is supported by the Novo Nordisk Foundation, Open Philanthropy and the Bill & Melinda Gates Foundation. The goal is to explore prioritized virus groups, identify therapeutic targets in three of these virus groups, and develop compounds to Phase I.
The German Fraunhofer Society opened a site for Immunology, Infection and Pandemic Control in May 2022, partnering with the University of Munich, the University Hospital and Roche.
The Antiviral Program for Pandemics of the U.S.
In 2021, the U.S. government is providing $3.2 billion for collaborative projects with academic institutions and companies to establish an Antiviral Drug Discovery Centers for Pathogens of Pandemic Concern, with the goal of developing therapeutics against multiple virus families.
Center for Pandemic Vaccines and Therapeutics (ZEPAI).
Established by the German Federal Ministry of Health at the Paul Ehrlich Institute, ZEPAI aims to build an infrastructure to provide vaccines and therapeutics to the population as quickly as possible. To this end, a pool of interdisciplinary experts is being established with expertise in production, logistics, infectiology, communications and public health care. Digital data collection and monitoring structures will be created to optimize planning and logistics. This will draw on the expertise of the companies with which the German government concluded pandemic preparedness contracts in May 2022.
Pandemic preparedness contracts
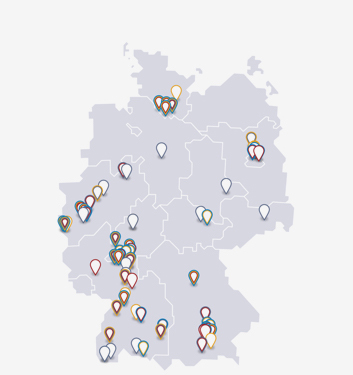
The May 2022 contracts between the federal government and BioNTech, CureVac, Wacker/CordenPharma, Celonic and IDT Biologika commit the companies to deploy production capacity for mRNA-, vector- and protein-based vaccines such that they can produce and deliver vaccines against the pathogen in question within months. The total capacity far exceeds Germany's own requirements.
Companies and consortia with which the German government has entered into pandemic preparedness agreements include
- BioNTech (mRNA vaccine)
- CureVac/GSK (mRNA vaccine)
- Wacker/CordenPharma (mRNA vaccine)
- Celonic (protein-based vaccine)
- IDT Biologika (vector vaccine)
The research-based pharmaceutical industry
In response to the pandemic, the industry has now developed a double-digit number of vaccines and therapeutics, the first of which was approved in December 2020. Additional agents against other pathogens are in development.
Awarded: Future Insight Prize for a Pandemic Early Warning System
The earlier a new pandemic is detected, the better the chances of containing it. Early warning systems are therefore of great importance. Merck KGaA has therefore announced the Future Insight Prize 2023 for the development of such an early warning system for pandemics. This prize, which is awarded annually for changing future-relevant developments, is endowed with 1,000,000 euros.
Notwithstanding the government initiatives and investments in research, their international coordination and the development of infrastructures that have been underway for two years, the role of industry is essential. For example, a new generation of vaccines has emerged based on mRNA technology developed over the past 20 years. An essential prerequisite for this was also the use of venture capital with a high risk of total loss. Furthermore, the safe production of vaccines and therapeutics as well as the scaling of production capacities and logistical expertise are among the indispensable core competencies of the medicine and diagnostics industry. For this private investment,