X-TEND
Xolair - Therapie-Nachverfolgung der abgeschlosse-nen Anwendungsbeobachtungen X-PERTISE und X-CLUSIVE
Titel der Studie/Acronym
X-TEND
Xolair - Therapie-Nachverfolgung der abgeschlosse-nen Anwendungsbeobachtungen X-PERTISE und X-CLUSIVE
Zielsetzung/Fragestellung
X-TEND ist eine nicht-interventionelle Follow-up Studie von Omalizumab bei Patienten ≥12 Jahren und verfolgt mehrere Ziele:
• Untersuchung der Anwendung von Xolair® über mehrere Jahre (Frequenz der Applikati-on, Dosis, Therapieunterbrechungen bzw. Theapieabbrüche)
• Evaluation von therapiebedingten Veränderungen des Krankheitsverlaufs, der Lebens-qualität und der Allergensensitivität (sofern vorhanden).
• Generierung von Daten zu Effektivität und Verträglichkeit der Therapie über mehrere Jahre
Indikation
- schweres persistierendes allergisches Asthma
Wirkstoff
- Omalizumab (deutsch)
Handelsname(n)
Xolair
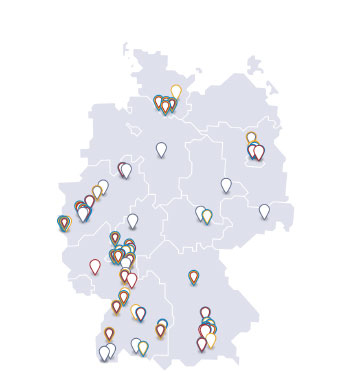
Geplante Anzahl vorgesehener Studienzentren: für die Untersuchung insgesamt
200
Geplante Patientenzahl: für die Untersuchung insgesamt
200
Kontaktperson
Müller, Alfons
Phase IV Manager NIS
Novartis Pharma GmbH
Roonstr. 25
90429 Nürnberg
Deutschland
Telefon: 0911/273-12897
Telefax: 0911/273-15897
Unternehmen
Novartis Pharma GmbH
Roonstr. 25
90429 Nürnberg
Deutschland
Stand der Information
14.06.2012
Status der Studie
Studie bereits abgeschlossen
Zusammenfassung der Ergebnisse
Methodologie
The study included a current visit and comparisons to baseline data obtained during the X-CLUSIVE and X-PERTISE studies.
Only diagnostic measures and medically indicated examinations under daily practice routine were documented. No intervention in the therapeutic decisions of the investigator was allowed. Xolair® was prescribed in the usual manner in accordance with the summary of product characteristics. No additional diagnostic or monitoring procedures had to be applied to the patients. Patients were included in the study only after they had signed an informed consent form.
Analysierte Anzahl der Patienten
106
Diagnose und Einschlußkriterium
Patients who participated in the non-interventional studies X-CLUSIVE and X-PERTISE, who were at least 12 years of age and for whom at least one follow-up was documented in order to study the effect of Xolair® therapy over several years. As many patients of X-CLUSIVE and X-PERTISE as possible were to be included in X-TEND; the maximum patient potential out of the two previous studies was 475 patients.
Wirkliche Dauer der Studie
13 Monate
Wirksamkeit unter Alltagsbedingungen
Allergy symptoms and disease consequences were recorded, specifically any serious asthma exacerbations during the preceding 12 months, asthma symptoms, lung function (current or most recent FEV1 value) and the number of days missed at school or work. Moreover, the current asthma medication and dose were recorded.
Sicherheit
The evaluation of safety was based on the incidence and profile of adverse events in this study
Andere
Patients also had to fill in a quality of life questionnaire and physicians evaluated the safety and efficacy of the current treatment compared to the beginning of the X-CLUSIVE and X-PERTISE studies and recorded any adverse event.
Methoden
The statistical evaluation was done in a purely descriptive manner. The output tables were prepared using the statistical software program SAS® Version 9.2 for Windows. For categorical data including categories of continuous data, frequency tables were prepared. In addition, continuous data were categorized in a clinically meaningful way. Multiple response data are presented as distribution of single entries. For quantitative (continuous) data, the parameters for statistical distribution (Mean, SD, Minimum, Median, Maximum, P5, P25, P75, P95, Non-Missing, Missing) were calculated.
Ergebnisse zur Wirksamkeit unter Alltagsbedingungen
Of the 106 patients included in this study, 46 had participated in X-CLUSIVE and 60 in X-PERTISE study. Overall, this study included more female (69 patients; 65.1%) than male patients (37 patients; 34.9%). The overall mean age was 48.9 ± 16.5 years. The overall mean weight was 80.8 ± 17.97 kg. The majority of patients were non-smokers (88; 83.0%), none of the patients smoked at the time of the visit, but 16 were former smokers (15.1%). Almost all patients (104; 98.1%) were still treated in the same practice as during the previous study, only 2 patients (1.9%) were not.
The mean age at therapy start of the previous study was similar between the two patient groups (X-CLUSIVE: 44.2 ± 18.22 years; X-PERTISE: 43.7 ± 15.28 years) and 43.9 ± 16.6 years overall.
The mean IgE level overall was 273.6 ± 210.38 IE/ml at the beginning of therapy (X-CLUSIVE: 277.7 ± 220.42 IE/ml; X-PERTISE: 270.7 ± 204.36 IE/ml. The mean 4-week dose of Xolair® was 389.4 ± 185.2 mg overall and very similar between patients recruited from both previous studies (X-CLUSIVE: 383.3 ± 190.69 mg; X-PERTISE: 394.1 ± 182.44 mg).
On average, patients had received their first dose of Xolair® 5.0 ± 0.5 years before the beginning of the X-TEND study. At the beginning of this non-interventional follow-up study, half of the patients (53; 50.0%) were still receiving Xolair® therapy, the therapy was discontinued for 49 patients (46.2%) and data on therapy status were missing for 4 patients (3.8%).
The mean duration of therapy was 1366.7 ± 636.99 days. On average, patients were exposed to Xolair® for 1252.5 ± 617.79 days. During the observation period from the start of therapy until the current visit, patients were not exposed to the drug for 571.8 ± 606.91 days. The mean Xolair® dose per 4 weeks was 412.8 ± 267.79 mg.
The large majority of patients (91; 85.9%) received inhalative corticosteroids in a fixed combination with long-acting beta2 agonists. More than half of the patients (60; 56.6%) received short-acting inhalative beta2 agonists. Slightly more than a third received leukotriene receptor antagonists (40 patients; 37.7%) or theophylline (39 patients; 36.8%).
The most frequently observed concomitant disease was allergic rhinitis/rhinoconjunctivitis in 28 patients (26.4%), followed by animal hair allergy in 27 patients (25.5%).
The most commonly observed sensitivity across all studies was to mites. While the majority of patients was sensitive to mites both at the beginning of the preceding study (X-CLUSIVE: 37 patients; 80.4%; X-PERTISE: 46 patients; 76.7%) and in this study (65 patients; 61.3%), the percentage of mite-sensitive patients was lower in the current study than in the previous ones. Other common sensitivities were observed to animal hair, grasses and early-blooming trees. All sensitivities observed were lower in the X-TEND studies than in the previous studies. Of the 106 patients, 7.5% had more sensitivities at the time of X-TEND compared to the beginning of the preceding studies. Fewer sensitivities than pre-study were reported for 50.9% and no change was reported in the number of sensitivities for 41.5% of patients.
Compared to the previous study, the number of patients experiencing frequent asthma symptoms during the day or night decreased strongly from 98.3% to 3.3% and 95.0% to 1.7%, respectively. FEV1 increased between the initial and current visit. The mean difference in FEV1 volume between the initial and current visits was 0.4 ± 0.64 L, in predicted FEV1 the mean difference was 12.6 ± 15.69%. On average, patients experienced 4.8 ± 10.45 severe asthma exacerbations in the 12 months before start of therapy in X-PERTISE. The number of exacerbations per 12 months had decreased about ten-fold at the start of X-TEND when patients had experienced 0.4 ± 0.99 exacerbations during the preceding 12 months.
While at the initial X-PERTISE visit, patients were absent from work or school for 15.0 ± 52.41 days within 12 months, they only missed 0.7 ± 3.55 days during the 12 months before inclusion into X-TEND.
Physicians were asked to perform a global evaluation of treatment effectiveness (GETE) for each patient with regard to asthma symptoms compared to the start of treatment in X-CLUSIVE or X-PERTISE. For patients with ongoing therapy, the effectiveness was “excellent” or “good” in the vast majority of patients (83.0%), “moderate” in 5.7% and “poor” or “worsening” in no patients. On the other hand, effectiveness of current treatment was “excellent” or “good” in only 46.9% of patients with discontinued therapy, “moderate” in 14.3% and “poor” or “worsening” in 24.5% of these patients.
Ergebnisse zur Sicherheit
During this follow-up study, a total of 66 AEs were documented in 25 of 106 patients (23.6%). In 12 patients, a non-serious adverse event with no or only improbable relationship to the study medication was reported. A non-serious adverse drug reaction (nsADR) was documented in 12 patients, i.e. the relationship to treatment was assessed as certain, probable, possible, not assessable, or missing. For 8 patients, at least 1 event met the criteria for a serious adverse event (SAE). No serious adverse drug reactions (SADR) were observed in this study. No patients died during this study.
Patients experienced non-serious adverse events and adverse drug reactions most frequently in the System Organ Class (SOC) Immune System Disorders, followed by Respiratory, thoracic and mediastinal disorders. Patients had SAEs most frequently in the SOC Respiratory, thoracic and mediastinal disorders, followed by Investigations. At the PT level, most patients reported asthma, followed by allergy to animal and forced expiratory volume decreased.
Ergebnisse zu anderen Parametern
Comparing the patients’ answers on a quality of life questionnaire between the initial X-PERTISE visit and the current X-TEND visit, there was a clear shift in patients’ answers from reporting more frequent asthma-related problems at the initial X-PERTISE visit to fewer problems at the current visit. The percentage of patients who reported the respective symptoms “always”, “usually” or “often”, was higher at the initial X-PERTISE visit than the current X-TEND visit. Conversely, the percentage of patients who stated that they “rarely”, “almost never”, “never” had the respective symptom was higher in the current X-TEND visit than at the initial X-PERTISE visit. The mean quality of life was 3.0 ± 0.79 at the initial visit and increased to 4.9 ± 1.52 at the current visit overall.
Schlussfolgerungen
On average, patients had received their first dose of Xolair® 5.0 ± 0.5 years before the beginning of the X-TEND study. At the beginning of this non-interventional follow-up study, half of the patients (53; 50.0%) were still on Xolair® therapy.
Sensitivities to allergens tended to be lower in the X-TEND study than in the previous studies. Improvement compared to the previous studies was also seen for the number of patients experiencing frequent asthma symptoms, the number of exacerbations per 12 months and the number of days absent from work or school. This indicated long-term efficacy of Xolair® therapy.
In the physician’s global evaluation of treatment effectiveness (GETE) for each patient with regard to asthma symptoms compared to the start of treatment in X-CLUSIVE or X-PERTISE the effectiveness was rated better for patients with ongoing therapy than for patients with discontinued therapy.
Based on the miniAQLQ patients reported fewer asthma-related problems than in the previous study and quality of life was considered better.
The AE profile seen in this study was in line with earlier findings