Supply bottlenecks for pharmaceuticals: Causes, consequences and solutions
Supply bottlenecks for medicines are a challenge for the healthcare system. The causes of supply problems are varied and affect patients in different areas.

IW study on supply chains:
Whether production bottlenecks, global dependencies or increasing demand: the complexity of supply chains often makes quick solutions difficult. The German Association of Research-Based Pharmaceutical Companies (vfa) explains the background and highlights concrete measures with a five-point plan to ensure security of supply in the long term.
The most important questions and answers
Which medicines are currently in short supply?

Supply bottlenecks for medicines have been a reliable feature of the German healthcare system since the coronavirus pandemic at the latest. A breast cancer drug, fever syrups for children, various vaccines and antibiotics - the list is always dynamic. The severity of such bottlenecks depends on the drug in question, the availability of alternatives with the same active ingredient or therapeutic alternatives and the severity of the illness being treated.
On the websites of the Federal Institute for Drugs and Medical Devices (BfArM), the Paul Ehrlich Institute (PEI) and also the European Medicines Agency (EMA), current or announced supply shortages of medicinal products are published on a daily basis. Of particular importance at present are the supply shortages for sterile saline solution and for pediatric antibiotics, whereby the latter are available to a much greater extent than in previous winters. Another supply shortage concerns atomoxetine-containing medicines for the treatment of attention deficit/hyperactivity disorder (ADHD), which was caused by a quality shortage. The manufacturer affected by the quality shortage supplies atomoxetine-containing medicinal products to various marketing authorization holders, which together account for around 80 percent of the market volume for medicinal products containing this active ingredient in Germany.
What alternative options are there, or what is the difference between a supply bottleneck and a supply shortage?

Alternative treatment options exist for most of the medicines for which a shortage is currently reported. Often, the supply shortage has no impact on patients, as they receive the same active ingredient in the same dosage, only the manufacturer of the medicine is different. This is usually the case when it comes to generic active ingredients that are manufactured and distributed by a large number of market participants. A restriction in treatment rarely occurs in these cases.
More serious are bottlenecks where only individual manufacturers serve the market, so that a large market share is affected in the event of a supply shortage. In these cases, such as the current supply shortage of atomoxetine-containing medicines, there are no or too few manufacturers available who can adequately compensate for the lost market share; the supply of medicines with the corresponding active ingredient is then not covered. However, the supply bottleneck for atomoxetine does not have a serious impact on supply, as only four percent of ADHD patients in Germany are treated with atomoxetine. As other active substances are available for this area of application, the supply can be maintained throughout the entire period of the shortage by switching to medication with other active substances. The two cases mentioned above are referred to as supply bottlenecks.
 In recent years, however, there have also been cases in which an adequate supply for serious illnesses could no longer be guaranteed. This situation can occur if a patent-protected drug is affected for which there are no alternatives with the same active ingredient. The new prophylaxis against RSV is such a case. The high demand for prophylaxis for the immunization of newborns cannot be fully met with the current production capacities. Due to the lack of alternatives, there is an undersupply that cannot be compensated for in the German market.
In recent years, however, there have also been cases in which an adequate supply for serious illnesses could no longer be guaranteed. This situation can occur if a patent-protected drug is affected for which there are no alternatives with the same active ingredient. The new prophylaxis against RSV is such a case. The high demand for prophylaxis for the immunization of newborns cannot be fully met with the current production capacities. Due to the lack of alternatives, there is an undersupply that cannot be compensated for in the German market.
In such cases, the German Medicines Act provides for the possibility of the BMG announcing a supply shortage (§79 (5) AMG). Once the supply shortage has been announced, the state authorities are free to allow the import and distribution of the medicine in question from abroad (even outside the EU) and thus bridge the shortage. In order to give all affected stakeholders the necessary reaction time, it is particularly important to notify the responsible higher authorities (i.e. BfArM or PEI) of an anticipated shortage at an early stage. In the case of RSV prophylaxis, this helped to take the necessary measures before the drug was no longer available.
This possibility of publicizing a supply shortage can also be used if several marketing authorization holders of medicinal products with the same active ingredient are affected by a shortage, so that there are too few packages of the active ingredient in question available overall; or if this even applies to medicinal products of an entire active ingredient group. This was observed on a large scale in the winter of 2022/2023, when the number of infections was unusually high compared to previous years.
As a result, the supply of antibiotics, especially for children, was severely restricted for months and could only be stabilized through imports. However, the bottleneck was exacerbated by uncontrolled stockpiling. Confidence in the security of supply therefore also plays a key role in combating supply bottlenecks. For the current supply shortage of sodium chloride solutions, the supply shortage was also announced in late summer 2024 in order to be able to meet the ongoing high demand.
Due to its integration into the EU and the numerous European initiatives to prevent and mitigate supply bottlenecks, it is not sensible to view the supply situation in Germany in isolation. Efforts should therefore be made to harmonize national and European processes using existing resources.
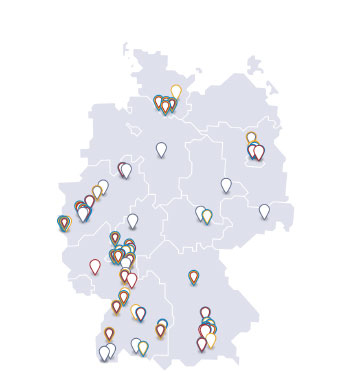
Where are the drugs in short supply mainly produced?

When it comes to supply bottlenecks for pharmaceuticals, it quickly becomes clear that dependence on China and India is having a negative impact on the availability of medicines in Germany. The trend towards relocating pharmaceutical production to the Far East continues unabated. China and India supply a large proportion of the required quantities of active ingredients and finished medicinal products worldwide, including antibiotics (german).
In Germany and Europe, only a few production facilities are still available for antibiotics, and their capacities cannot meet European demand. While this trend applies to many generic active ingredients, the vast majority of innovative medicines and vaccines are still manufactured in Europe and the USA. In the case of innovative pharmaceuticals, there is also a greater resilience of supply chains and therefore fewer supply bottlenecks. This is due to a greater diversification of suppliers and, above all, larger safety stocks.
What are the causes of this shortage?

The reasons for supply bottlenecks are varied and range from problems in the manufacture of active ingredients to a lack of production capacity and missing or faulty packaging materials. Due to the highly regulated pharmaceutical market, even small deviations in the manufacturing process or in quality characteristics are considered a reason for a delay in market supply, even if the deviations have no influence on the quality of the drug. If, for example, as in the case of sodium chloride solution, a packaging material is not available, the medicinal product cannot be manufactured in accordance with the approval, even if an alternative packaging material is available.
If problems occur in the production of the active ingredient or the end product, it is also not possible to fall back on an alternative manufacturer unless this has already been qualified in advance. In addition, many production facilities are working at full capacity, meaning that increases in demand cannot usually be met with additional production at short notice. The shortage of skilled workers, which is also a limiting factor for productivity in pharmaceutical production facilities, makes the situation even more difficult.
New national and international legislation can also lead to the need for changes in production or changes in profitability. For example, there is currently concern about developments regarding the PFAS ban, the Packaging and Packaging Waste Regulations (PPWR) or the Urban Wastewater Treatment Directive (UWWTD), but changes in Good Manufacturing Practice (GMP) guidelines can also make far-reaching, time-consuming and cost-intensive adjustments necessary.
Five-point plan
How supply bottlenecks for pharmaceuticals can be resolved
The stable supply of medicines is a central task for our healthcare system. However, supply bottlenecks - triggered, for example, by global crises such as the coronavirus pandemic or geopolitical conflicts - pose a significant challenge. Shortages can have serious consequences for patients, especially when it comes to innovative medicines without alternatives. With a five-point plan, the vfa is making proposals to solve these problems sustainably.
1. Establishing early warning systems for supply chains
Pharmaceutical supply chains are complex. An early warning system could identify problems at an early stage and enable countermeasures to be taken. The federal authority BfArM is already working on expanding and using existing databases to avoid critical bottlenecks. There are also projects at EU level, such as CHESSMEN, which aim to create standardized monitoring tools. The possibilities of big data and artificial intelligence offer great opportunities to systematically tap into new data sets - for example from SecurPharm.
2. Putting supply chains to the test
Stress tests can show how vulnerable supply chains and production networks are. The EU and other countries use such tests to identify risks and reduce dependencies. The pharmaceutical industry should be incentivized to diversify its sources of supply and make its production more resilient.
3. Taking a close look at stockpiling
Expanded warehousing is often seen as a solution, but it comes with challenges. Storage costs and capital expenditure can be high. Instead of large central warehouses, better use of existing stocks would be an effective solution, supported by an efficient early warning system.
4. Building up reserve capacities
Germany is a leading location for innovative pharmaceuticals. This strength should be used to build up reserve capacities. Flexible production networks and harmonized regulations between the EU and the USA could minimize bottlenecks in crises. At the same time, insurance models similar to those used in the fight against the pandemic could help to maintain production capacities.
5. Promoting innovation and technological leadership
A strong innovation network is essential - also to maintain technological sovereignty. Germany plays an important role in the European and global healthcare market. Better conditions for research and production - for example through patent protection, digital security and innovation clusters - can minimize technological risks and strengthen competitiveness.
Outlook
The vfa is committed to ensuring the supply of medicines at national and international level. The five-point plan offers pragmatic and future-oriented solutions to avoid supply bottlenecks and strengthen the resilience of the healthcare system.
vfa podcast #MacroScope on supply bottlenecks for medicines (german)
Download & Streaming
Follow the vfa's MacroScope podcast free of charge via these platforms:
Spotify |Apple Podcasts | Soundcloud | Amazon Music | Deezer | vfa Podcasts