Gender differences in pharmaceutical research
Drugs intended for men and women are also tested with men and women. This is required by the regulatory authorities and German law. The study results for both sexes are compared and are also included in the early benefit assessment that every new drug must undergo in Germany.

If, on the other hand, a drug is studied with only one sex, it also receives approval only for that sex. For this reason, some drugs for osteoporosis and breast cancer have been approved only for women, although in rare cases these diseases can also affect men - for example, in the case of breast cancer in this country, about 500 men versus 70,000 women per year. Another drug, for chronic constipation, was initially approved only for women; approval for men followed only after it had also been tested with enough men through further studies.(1)
The testing of drugs with humans prior to approval takes place in three phases:
- in Phase I in studies with a small number of healthy subjects
- in phase II in studies with a small number of patients
- in phase III in studies with many patients
Women and girls of reproductive age interested in participating must have a proven record of not being pregnant and must commit to reliable contraception - this applies to both healthy individuals and those with the disease. As a rule, contraception using two methods at the same time is required. Companies have a great interest in ensuring that both patients and female patients participate in the studies, because the faster they succeed in gathering the necessary number of participants, the faster drug development progresses.
Only the very first studies with a drug usually require only healthy male participants. These are studies in which not the effect, but first of all the "behavior" of the new active substance in the body must be investigated; and this in the simplest case, i.e. without the influence of hormonal fluctuations or hormonal contraceptives. This is most likely to be realized with men. However, the results must subsequently be verified with women. Accordingly, in the sum of all Phase I studies for a drug, a female part of 10 to 40 percent can be found.
In the studies with patients in phases II and III, however, 30 to 80 percent are female participants (70 to 20 percent male participants) if the disease occurs in both sexes.
Whether there are differences in the efficacy or tolerability of a new drug in women and men can be determined primarily in the phase III studies, because many more patients participate here than in the previous phases. It is not necessary for the same number of men and women to participate. All that is necessary for the comparison is that a sufficiently large number of treatments can be evaluated from each sex; and this is the case.
As a rule, sufficiently equal ...
What emerges from the gender-specific evaluation of the studies leads to an overall picture that includes a rule case and a few exceptions. First, about the rule case:
In drug trials, statistical differences can indeed often be found between women and men when it comes to the mean concentration and residence time of active ingredients in the blood. However, these differences are almost always smaller than the individual differences from person to person. In other words, whether one is fat or thin, trained or untrained, whether one has young or old kidneys, whether one smokes or not - all this changes the behavior of a drug in the body more than gender.
In addition, pharmaceutical researchers have usually succeeded in developing drugs whose effect and side effects are unaffected by whether their concentration and retention time in the body are somewhat higher or somewhat lower. Their application therefore does not have to be different for each patient.
But there are drugs for which it is indeed important that the active ingredient concentration is precisely matched to the person being treated, possibly even changing according to the situation. Such is the case with insulin and some older anticoagulants used to prevent thrombosis and stroke (the vitamin K antagonists, often called "blood thinners"): The insulin dose is usually reset at each meal; the dose of the "blood thinners" is usually reset weekly. Any adjustment for gender that may be necessary is done at the same time.
... but there are exceptions
In some cases, studies have shown that there are gender-related differences:
- A preparation for hair loss (active ingredient: minoxidil) must be dosed differently for women and men. It is therefore offered in separate presentations for men and women.
- A hormone drug (active ingredient: follitropin) for the treatment of fertility disorders (egg or sperm maturation) must be dosed differently for men and women.
- A drug for constipation (active ingredient: prucalopride) should be dosed higher in men than in women.
- A drug for lipodystrophy (active ingredient: metreleptin) should be dosed higher in women than in men.
- A drug for adult growth disorders (active ingredient: somapacitan) is advised to have a higher starting dose for women treated with estrogen than for other women and men.
- A drug for osteoporosis (active ingredient: romosozumab) received approval only for women because it led to more severe side effects in studies in men.
- A drug for sleep disorders (active ingredient: zolpidem) must be dosed individually. In the USA, the starting point for determining the dose for men and women is a different value for women in each case.
Further research on sex differences in drug efficacy and tolerability is important to find more such exceptions.
Results of the gender-specific evaluation
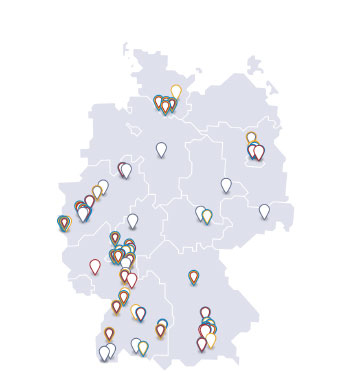
What the gender-specific evaluation of pivotal studies on new drugs has revealed can be found in the dossiers that manufacturers must submit to the Federal Joint Committee for their new drugs so that the committee can conduct an early benefit assessment (Module 4 in each case; subchapters 4.2.5.5 and 4.3.1). They are published on the website of the G-BA.
For the preparations evaluated and approved by the European regulatory authority EMA, corresponding results can be found under the keyword "gender" in the detailed European Public Assessment Reports (EPARs) available in English.
For older drugs, the package inserts and expert information (i.e., the expanded versions of the package inserts prepared for physicians and pharmacists) provide information on gender-specific differences, if such differences are to be taken into account in the treatment. In contrast, such information is usually not listed for drugs for which no relevant differences have been shown - but this does not mean that this has never been investigated.
Further information on the topic can be found in the vfa position paper "Consideration of women in drug research".
(1) Only in rare cases do regulatory authorities make an exception. For example, hemophilia A and B (two congenital clotting disorders) occur almost exclusively in boys and men. Accordingly, hardly any girls or women can participate in studies with drugs against it (see clinicaltrials.gov). The drugs - mostly concentrates with the respective missing clotting factor - have nevertheless also been approved for the few female sufferers.