ARCOS - Adult Risperdal® CONSTA® Outcome Study
Titel der Studie/Acronym
ARCOS - Adult Risperdal® CONSTA® Outcome Study
Zielsetzung/Fragestellung
Gewinnung von Langzeit-Daten zur Sicherheit, Verträglichkeit und Therapietreue zur Medikation unter der antipsychotischen Behandlung mit oralen Atypika und Depot-Atypika in der alltäglichen Behandlungsroutine von Patienten mit schizophrenen Psychosen. Zusätzlich werden Informationen zur Lebensqualität der Patienten - unter anderem hinsichtlich kognitiver Funktionen - sowie die Einstellung der Patienten zu der Behandlung dokumentiert
Indikation
- Schizophrenie
Wirkstoff
- Risperidon (deutsch)
Handelsname(n)
Risperdal CONSTA
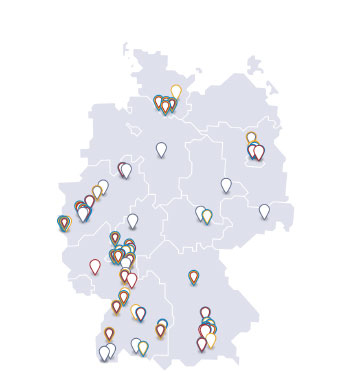
Geplante Anzahl vorgesehener Studienzentren: für die Untersuchung insgesamt
200
Geplante Patientenzahl: für die Untersuchung insgesamt
700
Kontaktperson
Hargarter, Ludger
Medical Development Manager
Janssen-Cilag GmbH
Johnson & Johnson Platz 1
41470 Neuss
Deutschland
Telefon: 02137 955 1240
Telefax: 02137 955 408
Unternehmen
Janssen-Cilag GmbH
Johnson & Johnson Platz 1
41470 Neuss
Deutschland
Stand der Information
15.07.2011
Status der Studie
Studie bereits abgeschlossen
Zusammenfassung der Ergebnisse
Methodologie
Non-interventional, prospective, two-arm; post-marketing surveillance study (phase IV)
Analysierte Anzahl der Patienten
746
Diagnose und Einschlußkriterium
• Diagnosis of schizophrenia (F20.x) according to ICD-10; severity of disease had to be lower or equal to ‘patient is markedly ill’ ( 5) based on the CGI-S Scale score at start of documentation;
• Indication for long-term treatment with an atypical antipsychotic;
• Change to oral treatment with an atypical antipsychotic (amisulpride, aripiprazole, olanzapine, quetiapine, ziprasidone or oral risperidone) or to intramuscular injection of RLAI at start of documentation
• Intended treatment concept was the use of only one single atypical antipsychotic.
Wirkliche Dauer der Studie
54 Monate
Wirksamkeit unter Alltagsbedingungen
Primary efficiency parameters were ‘retention rate’ (number of patients still remaining on the initially prescribed atypical antipsychotic medication at the end of documentation), and ‘retention survival time’ of the atypical antipsychotic in monotherapy.
Sicherheit
Documentation of adverse events and serious adverse events throughout the study period.
Andere
Additional outcome parameters were
- Current treatment with highly potent antipsychotics and use of additional psychotropic agents
- Judgment of compliance by the physician
- Health care utilization (relapse and hospitalization due to an underlying psychiatric disease)
- Documentation of adverse events (e.g. EPS)
- Assessment of psychopathology (PANSS)
- Assessment of global functioning (GAF)
- Assessment of disease severity (CGI-S) and changes of disease severity (CGI-C)
- Assessment of socioeconomic data
- Assessment of quality of life and attitude towards treatment (patient questionnaire)
- Assessment of cognitive functions (verbal fluency, digit span)
Methoden
Statistical analysis was planned to be exploratory. All data were summarized and analyzed by descriptive statistics using tabulation and graphs. All p-values and confidence intervals of inferential statistical methods are to be interpreted in the exploratory sense only.
The following treatment groups were defined for the statistical analysis:
• ‘RLAI’, all patients starting treatment with risperidone long-acting injectable (Risperdal® CONSTA®). This comprised ‘subgroup A’ (RLAI from start until end of documentation) and ‘subgroup B’ (RLAI at start of documentation but change of therapy during observation)
• ‘oAP (oral atypical antipsychotic)’, all patients starting treatment with an oral atypical antipsychotic. This comprised ‘subgroup C’ (oral atypical antipsychotic from start until end of documentation) and ‘subgroup D’ (oral atypical antipsychotic at start of documentation but change of therapy during observation).
The allocation to these subgroups was based on the documented data in the CRF.
Missing data were not replaced, but handled as ‘missing’ in the statistical evaluation. In case of premature termination, however, the last available observation after baseline was used for analysis (LOCF approach), if appropriate. Missing baseline data were not replaced.
Categorical data are presented in frequency tables using counts and percentages based on the total number of patients in the respective analysis set unless otherwise specified. Cross tabulation vs. baseline by study visit is provided, if appropriate. Standard descriptive summary statistics are calculated for continuous and quasi-continuous variables: arithmetic mean, standard deviation, minimum value, lower quartile, median, upper quartile, maximum value, and number of non-missing values. Evaluation of relevant pre-post-changes within a group was done using adequate parametric or non-parametric tests for dependent samples (e.g. 1-sample t-test, Wilcoxon-test, χ2-test). The examination of differences between two or more than two (sub-)groups was conducted using adequate parametric or non-parametric tests for independent samples (e.g. 2-sample t-test, Mann-Whitney-U-test, Kruskal-Wallis statistic). Logistic regression analysis was used to assess the influence of one or more continuous or categorical explanatory variables on a single binary categorical outcome variable. The SAS LIFETEST procedure was used to compute nonparametric estimates of the survival distribution function according to the product-limit (Kaplan-Meier) method. In addition, the SAS PHREG procedure was used to perform regression analysis of survival data based on the Cox proportional hazards model. Cox’s model was used in the analysis of survival data to explain the effect of explanatory variables on survival time.
Ergebnisse zur Wirksamkeit unter Alltagsbedingungen
Baseline demographics
<tabelle>
<zeile>
<kopfspalte colspan='4'>Study Completion/Withdrawal Information</kopfspalte>
</zeile>
<zeile>
<feld></feld>
<feld><fett>Total</fett></feld>
<feld><fett>RLAI</fett></feld>
<feld><fett>oAP</fett></feld>
</zeile>
<zeile>
<feld></feld>
<feld></feld>
<feld><fett>n (%)</fett></feld>
<feld></feld>
</zeile>
<zeile>
<feld><fett>All patients documented</fett></feld>
<feld><fett>750</fett></feld>
<feld>-</feld>
<feld>-</feld>
</zeile>
<zeile>
<feld>Patients without information regarding treatment group</feld>
<feld>4</feld>
<feld>—</feld>
<feld>—</feld>
</zeile>
<zeile>
<feld><fett>All patients treated (‘intent-to-treat analysis set’)</fett></feld>
<feld><fett>746 (100.0)</fett></feld>
<feld><fett>478 (100.0)</fett></feld>
<feld><fett>268 (100.0)</fett></feld>
</zeile>
<zeile>
<feld>Patients treated but not evaluable for ‘retention rate’</feld>
<feld>124 (16.6)</feld>
<feld>77 (16.1)</feld>
<feld>47 (17.5)</feld>
</zeile>
<zeile>
<feld>
<fett>All patients evaluable for retention rate</fett>
(high potency neuroleptic medication as monotherapy, and calculated ‘retention survival time’ > 0)
</feld>
<feld>622 (83.4)</feld>
<feld>401 (83.9)</feld>
<feld>221 (82.5)</feld>
</zeile>
<zeile>
<feld><fett>All patients with other major protocol violations</fett></feld>
<feld><fett>20 (2.7)</fett></feld>
<feld><fett>11 (2.3)</fett></feld>
<feld><fett>9 (3.4)</fett></feld>
</zeile>
<zeile>
<feld><fett>Per-Protocol analysis set</fett></feld>
<feld><fett>602 (80.7)</fett></feld>
<feld><fett>390 (81.6)</fett></feld>
<feld><fett>212 (79.1)</fett></feld>
</zeile>
<zeile>
<feld><fett>Premature termination</fett></feld>
<feld><fett>408 (54.7)</fett></feld>
<feld><fett>256 (53.6)</fett></feld>
<feld><fett>152 (56.7)</fett></feld>
</zeile>
<zeile>
<feld><liste><element>Treatment change: insufficient eff. for positive symptoms</element></liste></feld>
<feld>21 (2.8)</feld>
<feld>16 (3.3)</feld>
<feld>5 (1.9)</feld>
</zeile>
<zeile>
<feld><liste><element>Treatment change: insufficient eff. for negative symptoms</element></liste></feld>
<feld>5 (0.7)</feld>
<feld>4 (0.8)</feld>
<feld>1 (0.4)</feld>
</zeile>
<zeile>
<feld><liste><element>Treatment change: treatment change: Lack of tolerability</element></liste></feld>
<feld>10 (1.3)</feld>
<feld>7 (1.5)</feld>
<feld>3 (1.1)</feld>
</zeile>
<zeile>
<feld><liste><element>Treatment change: wish of patient/caregiver/relative</element></liste></feld>
<feld>30 (4.0)</feld>
<feld>24 (5.0)</feld>
<feld>6 (2.2)</feld>
</zeile>
<zeile>
<feld><liste><element>Stop of trial: wish of patient/caregiver/relative</element></liste></feld>
<feld>43 (5.8)</feld>
<feld>27 (5.6)</feld>
<feld>16 (6.0)</feld>
</zeile>
<zeile>
<feld><liste><element>Other reasons (e.g., missed study dates)</element></liste></feld>
<feld>336 (45.0)</feld>
<feld>205 (42.9)</feld>
<feld>131 (48.9)</feld>
</zeile>
<zeile>
<feld><liste><element>Missing</element></liste></feld>
<feld>6 (0.8)</feld>
<feld>4 (0.8)</feld>
<feld>2 (0.7)</feld>
</zeile>
<zeile>
<feld><fett>Completed</fett></feld>
<feld><fett>338 (45.3)</fett></feld>
<feld><fett>222 (46.4)</fett></feld>
<feld><fett>116 (43.3)</fett></feld>
</zeile>
<zeile>
<feld colspan='4'>RLAI: risperidone long- acting injectable (Risperdal® CONSTA®), subgroups A/B; oAP: oral atypical antipsychotics, subgroups C/D</feld>
</zeile>
</tabelle>
Treatment groups (RLAI; subgroups A/B and oAP; subgroups C/D) did not differ significantly in terms of baseline characteristics but patients treated with RLAI were more likely to be male, non-compliant, substance abuser, and had significantly higher levels of psychotic symptoms and disease severity, poorer psychosocial functioning (GAF, days unable to work), and poorer cognitive function, compared to patients treated with oral antipsychotics. 107 patients were identified as having a history of poor adherence (RLAI: n=84; oral: n=23) with previous antipsychotic treatment.
Efficacy results:
The following table shows the results of efficiency criteria for the two main treatment groups (ITT analysis group; mainly arithmetic means and standard deviation). In several parameters, improvements were seen for all treatment groups. They were generally more pronounced in the subgroups A and C, i.e. in patients without change of medication during the study course. However, no relevant differences in efficiency were found when comparing patients treated with RLAI (Risperdal® CONSTA®) and all patients treated with oral atypical antipsychotics.
<tabelle>
<zeile>
<feld></feld>
<feld colspan='2'><fett>RLAI n=478</fett></feld>
<feld colspan='2'><fett>oAP n=268</fett></feld>
</zeile>
<zeile>
<feld><fett>Retention rate<fussnote>N patients remaining on the initially prescribed medication from start until end of the study; 2-sided p-value for the between-group comparison: p = 0.4825;</fussnote> [n patients (%)]</fett></feld>
<feld colspan='2'>145/401 (36.2%)</feld>
<feld colspan='2'>73/221 (33.0%)</feld>
</zeile>
<zeile>
<feld><fett>Retention survival time<fussnote>Time from start of therapy until first discontinuation of atypical antipsychotic monotherapy from study start.</fussnote> [days ±SD]</fett></feld>
<feld colspan='2'>393. 7 (14.1)*</feld>
<feld colspan='2'>392.2 (19.6)*</feld>
</zeile>
<zeile>
<feld><fett>Number of relapses</fett></feld>
<feld colspan='2'>0.4 (0.7)**</feld>
<feld colspan='2'>0.3 (0.7)**</feld>
</zeile>
<zeile>
<feld>Patients with relapses [n (%)]</feld>
<feld colspan='2'>138/478 (28.9%)</feld>
<feld colspan='2'>73/268 (27.2)</feld>
</zeile>
<zeile>
<feld><fett>Time to first relapse [days ±SD]</fett></feld>
<feld colspan='2'>547.3 (12.5)*</feld>
<feld colspan='2'>485.4 (15.1)*</feld>
</zeile>
<zeile>
<feld><fett>Number of hospitalizations (SD)</fett></feld>
<feld colspan='2'>0.3 (0.6)**</feld>
<feld colspan='2'>0.3 (0.7)**</feld>
</zeile>
<zeile>
<feld>Days of hospitalization (SD)</feld>
<feld colspan='2'>57.1 (44.1)**</feld>
<feld colspan='2'>50.3 (37.7)**</feld>
</zeile>
<zeile>
<feld><fett></fett></feld>
<feld colspan='2'><fett>Mean (SD)</fett></feld>
<feld colspan='2'><fett>Mean (SD)</fett></feld>
</zeile>
<zeile>
<feld><fett></fett></feld>
<feld><fett>Month 0, V1</fett></feld>
<feld><fett>Month 24, V9</fett></feld>
<feld><fett>Month 0, V1</fett></feld>
<feld><fett>Month 24, V9</fett></feld>
</zeile>
<zeile>
<feld><fett>Extrapyramidal symptoms [pts]</fett></feld>
<feld>3.6 (4.7)</feld>
<feld>1.3 (3.1)</feld>
<feld>2.6 (4.2)</feld>
<feld>1.0 (2.1)</feld>
</zeile>
<zeile>
<feld><fett>PANSS total score [pts]</fett></feld>
<feld>87.3 (27.8)</feld>
<feld>61.0 (25.3)</feld>
<feld>80.2 (25.8)</feld>
<feld>56.4 (21.7)</feld>
</zeile>
<zeile>
<feld><fett>Global functioning [pts]</fett></feld>
<feld>52.3 (13.5)</feld>
<feld>65.1 (16.0)</feld>
<feld>56.3 (14.1)</feld>
<feld>68.0 (15.8)</feld>
</zeile>
<zeile>
<feld><fett>Severity of illness [pts]</fett></feld>
<feld>4.26 (0.68)</feld>
<feld>3.72 (1.09)</feld>
<feld>4.06 (0.71)</feld>
<feld>3.58 (1.01)</feld>
</zeile>
<zeile>
<feld><fett>Global improvement [pts]</fett></feld>
<feld>—</feld>
<feld>2.60 (1.22)</feld>
<feld>—</feld>
<feld>2.57 (1.18)</feld>
</zeile>
<zeile>
<feld><fett>Quality of life</fett></feld>
<feld colspan='2'></feld>
<feld colspan='2'></feld>
</zeile>
<zeile>
<feld>SWN-K sum score [pts]</feld>
<feld>76 (17)</feld>
<feld>85 (15)</feld>
<feld>77 (17)</feld>
<feld>86 (16)</feld>
</zeile>
<zeile>
<feld>WHO DAS II sum score [pts]</feld>
<feld>22 (7)</feld>
<feld>17 (7)</feld>
<feld>22 (8)</feld>
<feld>18 (7)</feld>
</zeile>
<zeile>
<feld>Satisfaction with therapy [pts]</feld>
<feld>35 (7)</feld>
<feld>39 (8)</feld>
<feld>36 (6)</feld>
<feld>41 (7)</feld>
</zeile>
<zeile>
<feld><fett>Sum score verbal fluency [pts]</fett></feld>
<feld>21.2 (9.6)</feld>
<feld>25.8 (10.9)</feld>
<feld>23.1 (9.4)</feld>
<feld>26.3 (11.6)</feld>
</zeile>
<zeile>
<feld><fett>Total sum score digit span [pts]</fett></feld>
<feld>11.4 (4.2)</feld>
<feld>13.0 (4.3)</feld>
<feld>12.6 (4.3)</feld>
<feld>13.7 (4.8)</feld>
</zeile>
<zeile>
<feld><fett>Days unable to work in last year</fett></feld>
<feld>123 (140)</feld>
<feld>64 (127)</feld>
<feld>97 (128)</feld>
<feld>42 (94)</feld>
</zeile>
<zeile>
<feld colspan='5'>
<fussnotenindex />
*): mean (standard error)
**): mean (SD);
pts.: points
<fett>Note</fett>: mean survival time/standard error tend to be underestimated as the longest survival time was censored
</zeile>
</tabelle>
Ergebnisse zur Sicherheit
Adverse events and serious adverse events were common in this study with a total of 2,702 AEs in 549/746 patients (73.6%), thereof 333 in 182/746 patients (24.4%) considered as SAEs. The rate of occurrence did not differ significantly when comparing patients with RLAI treatment with patients treated with oral atypical antipsychotics. However, clearly more SAEs occurred both in subgroup B (patients initially treated with RLAI and subsequent change of medication) and subgroup D (patients initially treated with oral atypical antipsychotics and subsequent change of medication) in contrast to patients of the subgroups A and C, who did not change their medication during the study. When comparing subgroup B and subgroup D, the rate of occurrence of SAEs was similar.
Causality was assessed as ‘very likely’ for 200 AEs, ‘probable’ for 345 AEs, and ‘possible’ for 775 AEs. 8 SAEs were considered to be ‘very likely’ related to study medication, 24 to be probably related, and 33 to be possibly related. Thus the majority of SAEs was considered not causally related to study medication intake.
4 patients died during the study and in 8 patients the outcome of 14 SAEs was assessed as ‘permanent damage’ in the sense of ongoing sequelae. All these cases were rated as being not related/doubtful related to study medication intake.
Patients in subgroup A (treated with RLAI during the entire study) had a lower increase in body weight compared to all other patients.
Ergebnisse zu anderen Parametern
Schlussfolgerungen
In this non-interventional study, patients benefited from study therapy as shown by analyzing the pre-defined efficiency parameters. Patients who received the same medication throughout the study (subgroups A and C) generally showed a better response compared to patients who were switched from their initially assigned antipsychotic.
Time to treatment discontinuation was numerically, but not significantly longer for patients treated with RLAI throughout the study (subgroup A) compared to patients treated with oAP throughout the study (subgroup C).
Post- hoc analysis of the data revealed that among the subset of patients with a history of poor compliance this difference was significant (unadjusted hazard ratio=0.42, p=.014; adjusted hazard ratio=0,35; p=0.0098). Symptom improvement was significantly better for patients on RLAI (subgroup A) as compared to oAP (subgroup C) on the Positive and Negative Syndrome Scale (PANSS) total score (p=.029), positive (p=.004) and negative (p=.023) subscores, respectively. At baseline, patients treated with RLAI were more likely to be male, non-compliant, substance abuser, and had significantly higher levels of psychotic symptoms and disease severity, poorer psychosocial functioning (GAF, days unable to work), and poorer cognitive function, compared to patients treated with oral antipsychotics. 107 patients were identified as having a history of poor adherence (RLAI: n=84; oral: n=23) with previous antipsychotic treatment. It has to be noted that poor response was one of the reasons to change medication during the observational period. Therefore, all patients with unsatisfactory results under treatment were prone to be found in the subgroups B and D, while the subgroups A and C were restricted to those patients showing a good response with their initial treatment. The same is true, when comparing rates of AEs: a high number of adverse events led to a change of medication, and thus patients in the subgroups A and C were automatically more likely to have lower rates of AEs reported. The overall rates of AEs and SAEs were similar for Risperdal® CONSTA® treated patients and patients treated with oral atypical antipsychotics.
Conclusion: In routine clinical practice, RLAI appears to be used more frequently in patients with more severe schizophrenia, substance abuse and poor adherence. The benefits of RLAI treatment compared to oAP seem to be most pronounced in a subset of patients with a history of poor adherence.