EPidemiologic evaluation Of patientS with Heart Failure with Preserved Systolic Function (EPOS)
- Register -
Titel der Studie/Acronym
EPidemiologic evaluation Of patientS with Heart Failure with Preserved Systolic Function (EPOS)
- Register -
Zielsetzung/Fragestellung
Wie groß ist der Anteil der Patienten, die sich beim niedergelassenen Kardiologen oder in einer internistischen/kardiologischen Klinikabteilung mit den Symptomen einer Herzinsuffizienz vorstellen, mit einer diastolischen Herzinsuffizienz?
Indikation
- diastolische Herzinsuffizienz
Wirkstoff
- ohne (deutsch)
Handelsname(n)
ohne
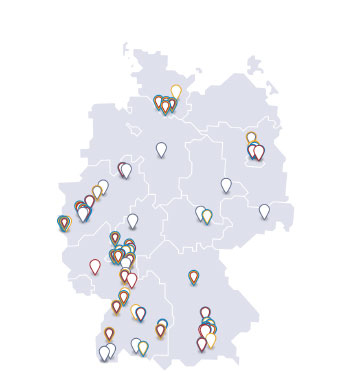
Geplante Anzahl vorgesehener Studienzentren: für die Untersuchung insgesamt
240
Geplante Patientenzahl: für die Untersuchung insgesamt
2400
Kontaktperson
Wörz, Karl
Leiter NIS-Management
Sanofi-Aventis Deutschland GmbH
Potsdamer Straße 8
10785 Berlin
Deutschland
Telefon: 069/305-80765
Telefax: 069/305-25730
Unternehmen
Sanofi-Aventis Deutschland GmbH
Potsdamer Strasse 8
10785 Berlin
Deutschland
Stand der Information
30.05.2011
Status der Studie
Studie bereits abgeschlossen
Zusammenfassung der Ergebnisse
Methodologie
vgl. abstract
Analysierte Anzahl der Patienten
1505
Diagnose und Einschlußkriterium
Background: Evidence suggests that diastolic heart failure is often not sufficiently diagnosed and medically treated. The register EPOS ( Epidemiologic evaluation Of patients with Heart Failure with Preserved Systolic Function) is the first prospective, community-based investigation to better characterise the incidence, diagnostic procedures and treatment of diastolic heart failure. This study included patients with clinical symptoms of heart failure. Primary issue was to evaluate among patients visiting a practice-based cardiologist or an internal medicine/cardiology hospital department due to heart failure the proportion of those patients suffering from diastolic heart failure. Secondary issue concerned the course of diagnostics, the current medical treatment, the concomitant diseases and their influences on pharmacotherapy.
Wirkliche Dauer der Studie
16 Monate
Wirksamkeit unter Alltagsbedingungen
vgl. abstract
Sicherheit
vgl. abstract
Andere
Patients: A total of 1,505 patients were included, 891 (59.2%) of them female and 612 (40.7%) male with a mean body weight of 82.2 kg and a mean height of 167.4 cm. Body Mass Index (BMI) averaged 29.3. The patients had a mean age of 68.9 years. An average blood pressure of 140.3/81.6 mmHg and a mean heart rate of 74.5 bpm were found.
Methoden
vgl. abstract
Ergebnisse zur Wirksamkeit unter Alltagsbedingungen
vgl. abstract
Ergebnisse zur Sicherheit
vgl. abstract
Ergebnisse zu anderen Parametern
Results: The degree of functional impairment was determined according to the NYHA-Classification. The majority of patients (61.4%) were placed in NYHA-class II, 33.7% in NYHA-class III und 4.9% in NYHA-class IV. According to the major symptom in heart failure 94% of the patients suffered from dyspnoea at cardiac stress and 67% showed reduced physical performance capacity. Almost one third of the patients were affected by fatigue/daily fatigue (32.3%), oedema (27.6%) and/or nycturia (27.0%). A minor proportion of patients suffered from palpitations (19.1%), dyspnoea at rest (14.2%), increase in body weight (13.6%), orthopnoea or paroxysmal nocturnal dyspnoea (12.8%) and/or nocturnal cough (7.3%). Among the examination findings oedema (25.8%) were predominant followed by respiratory rale (10.5%), tachycardia (9.2%) and/or carotid artery stenosis (9.0%).
The cardial anamnesis showed arterial hypertension in 82.6% of the patients (mean systolic blood pressure 148.6 mmHg, mean diastolic blood pressure 85.7 mmHg), coronary heart disease in 29.5%, atrial fibrillation in 25.5% (paroxysmal 40.6%, permanent 37.3%, persistent 19.3%), vitia in 22.3% (63.7% mitral valve insufficiency, 25.8% aortic valve insufficiency, 24.5% tricuspidal valve insufficiency, 19.1% aortic valve stenosis), „condition after cardiac surgery“ in 4.3%, cardiomyopathy in 9.5% (63.9% dilatative, 30.5% hypertrophic, 0.7% restrictive), myocardial infarction in 11.8%, condition after bypass surgery 8.6%, stroke/transient ischemic attack (TIA) in 6.1% /, peripheral vascular disease (PVD) in 5.2%.
Within the general anamnesis the following concomitant diseases were documented: hypercholesterinemia 51.9% (mean plasma cholesterol level 211.4 mg/dl), hypertriglyce¬ridemia 21.5% (mean plasma trigyceride level 204.6 mg/dl), renal insufficiency 41.3% (mean creatinine value 1.7 mg/dl; mean creatinine clearance 51,4 ml/min), microalbuminuria 2.0% (mean urinary albumin excretion 131.6 mg/l), type-1- or type-2-diabetes 30.4% (mean HbA1C-value 6.7%; therapy: insulin 29.5%, sulfonylurea derivates 19.5%, glitazones 6.8%, dietary management 20.8%), pulmonary diseases 21.3% (COPD 53.8%, asthma 10.9%, other pulmonary diseases 17.2%), sleep apnoea syndrome 3.2%, reduced physical fitness 22.5%, Smoker 30.0%. Results of hematology: mean Hb-value 13.3 g/dl.
Premedication received 93.9% of the patients, in detail: beta blockers 62.4%, diuretics 54.9%, ACE-inhibitors 47.7%, antiplatelet drugs 37.5, statines 33.5%, calcium blockers 24.1%, AT1-blockers 22.1%, oral anticoagulants 16.7%, nitrates 9.0%, digitalis 8.1%, aldosterone antagonists 6.8%, antidepressants 4.9%, fibrates 1,5%, renine inhibitors 1.0%.
Electrocardiography (ECG) was conducted in 98.5% of cases. The majority of patients (78.1%) showed sinus rhythm, in 16.5% atrial fibrillation was diagnosed and 12.4% showed ischemic signs or repolarisation disturbances. In 5.1% of the patients a pacemaker ECG was found. In 22.3% of cases hypertrophy was proven by means of the Sokolow index (mean value 2.1 mV).
Regarding the frequency of diagnostic methods used ECG and continuative echocardiographic methods were by far the most frequently ones with 98.5% and 98.7%, respectively. Almost ¾ of the patients (72.9%) were diagnosed via echocardiography and in almost half of the patients (43.6%) a tissue Doppler analysis was performed or biomarkers (47.1%) were determined. Only in few cases invasive hemodynamic methods (9.4%) and spiroergometry (3.6%) were applied.
The specific diagnosis led to some alterations in pharmacotherapy. The application of antidepressants (-0.9% points), fibrates (-0.6% points) und „other medications“ (-7,8% points) decreased. All other drugs were intended to increased use, particularly diuretics (+11.4% points) und ACE-inhibitors (+10.9% points), as well as statines (+6.3% points), aldosterone antagonists (+5.8% points), AT1-blockers (5.3% points) und beta blockers (+4.7% points).
The course of diagnostic procedures taken by the physicians was evaluated through the modified diagnostic algorithm of the European Society of Cardiology 2007. Due to the documented data within this algorithm the physicians concluded in 23.8% of the patients [95% CI: 0.22 – 0.26] Extracardial Reason (practice-based physicians: 27.1%, n = 1025; clinicians: 16.7%, n = 480), in 20.6% of the patients [95% CI: 0.19 – 0.23] Systolic Heart Failure (practice-based physicians: 15.4%, n = 1025; clinicians: 31.7%, n = 480) and in 54.1% of the patients [95% CI: 0.52 – 0.57] Diastolic Heart Failure/ Heart Failure With Normal Left Ventricular Systolic Function (practice-based physicians: 54.9%, n = 1025; clinicians: 52.3%, n = 480).
Schlussfolgerungen
vgl. abstract